Plant trauma may exert its effects by
mechanical forces, chemical injury or a hypersensitivity reaction. Crystalline keratopathy due to plant sap exposure was reported for the
first time in 1973 by Ellis1, who described needle-like crystals in
the corneal epithelium and stroma in a boy, who accidentally splashed his eyes
with the sap of Dieffenbachia, an
ornamental houseplant. These needle-like crystals or raphides2, are found within the leaves and stems of this
plant, and are composed of calcium
oxalate, which cause an explosive keratoconjunctivitis upon contact with
eyes.
The other species3,4 of plants
known to cause crystalline keratopathy are Arisaema,
Colocasia, Pinellia, Phylodendron,
and Alocasia, although raphides are
also found in other philodendron plants of the Araceae family, and may cause similar findings.2 The
more common cause of crystal deposition in the cornea is infectious crystalline
keratopathy, first reported in 1983 by Gorovoy5 et al in a corneal
transplant, attributed to stromal colonization of gram-positive cocci along a
suture tract. Subsequently, there have been numerous such cases, classically
described as branching, needle-like stromal crystals; associated most
frequently with penetrating keratoplasty, but also with incisional surgeries like
keratotomy, contact lens wear, chemical burns, and even topical anesthetic
abuse.6,7 Culprits identified are most commonly bacteria; Streptococcus viridians most often, but S. pneumoniae, Haemophilus aphrophilus,
Peptostreptococcus, Pseudomonas aeruginosa, and numerous others; but fungi
like Candida and Alternaria species have been isolated as well6.
Schnyder corneal
dystrophy, cystinosis, tyrosinemia, gout, Bietti crystalline dystrophy,
multiple myeloma, monoclonal gammopathy, gold, and drugs, are other causes of
corneal crystals8. Scant case reports of self-induced corneal
crystals can also be found, with one man admitting to injecting blue eyeshadow9
into his corneas. However, a crystalline traumatic cataract has never been
described before in literature. We report a case of crystalline keratopathy
with associated similar crystalline cataract as a result of tree sap injury,
decades prior to discovery.
CASE REPORT
A 51-year-old hospital
staff worker with no known comorbids presented in the outpatient department of
Fauji Foundation Hospital, which is a tertiary care teaching hospital,
affiliated with the Foundation University Medical College; with complaints of grittiness
and redness of the left eye for a few days. On examination, his visual acuity
was 6/6 in the right eye and 6/12 in the left; his symptoms were attributed to
an inflamed pterygium of the left eye. However, it was discovered on routine slit
lamp examination, that his left cornea had a sickle shaped distribution of
fine, iridescent, silvery crystals in a full thickness, paracentral corneal
scar extending from 5:30 to 8:30 o’clock (Figure 1 A-E).
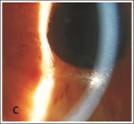

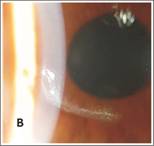
Fig. 1: A. Corneal crystals in a sickle shaped scar and sphincter damage
(white asterisks) B. Larger deposits on lateral illumination C. Full thickness
crystal deposition D. Inflamed pterygium (black asterisk) and brownish deposits
intermixed with crystals.
Brownish deposits were
also seen at some places intermixed with the crystals. This finding was
correlated by the patient, to a tree branch injury which occurred in 1991, twenty
seven years back, when he got hit accidentally, by an overhanging tree branch
while travelling on the roof of a large vehicle at night. He did not see the
tree in the dark and could not identify the type of tree; however, he did
recall some substance being instilled in his eye leading to severe inflammatory
symptoms. He was rushed to and admitted at that time in a local hospital and
was managed conservatively with topical and systemic antibiotics or steroids,
presumably, because he was unaware of the nature of the medicines and could not
recall their names. He denied self-medication or instillation of any chemical into
his eye. On further examination, he had a quiet anterior chamber, but iris
sphincter damage was visualized from 7 o’ clock to 8:45 o’ clock, with loss of
the pupillary ruff, and a hint of a localized cataract. Upon dilatation of
pupil, similar iridescent crystals were seen dispersed inside the localized
oval, traumatic cortical cataract at 5 o’ clock position (Figure 2).
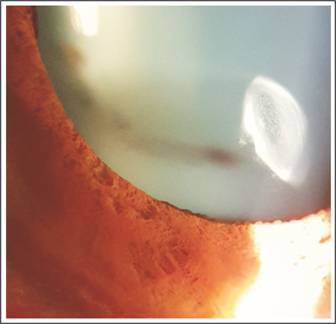
Fig. 2: Iridescent crystalline traumatic cortical cataract.
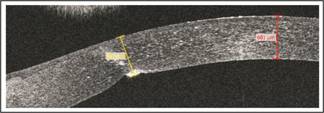
Fig. 3: Anterior segment OCT (AS-OCT) of the left cornea, showing the full
thickness scar measuring 652 µm, with refractile crystals dispersed in the
stroma. The central corneal thickness is 681 µm.
The rest of the lens was
clear. Anterior segment OCT (AS-OCT) was done which showed full thickness
corneal scar, with stromal dispersion of crystals (Figure 3), and the cortical
lenticular opacity with crystals as well (Figure 4).
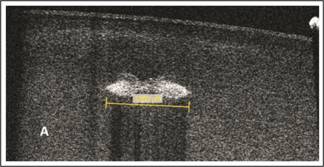
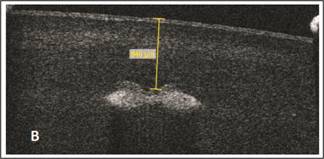
Fig. 4: A. AS-OCT of the lens showing the anterior cortical cataract (1095
µm in size), with interspersed crystals.
B. Cataract is located 840 µm from the anterior lens
capsule.
The fundus examination was normal. The
right was normal except for a mild pterygium. Intraocular pressures were 11 mm
Hg OD and 12 mm Hg OS. He was given topical tobramycin-dexamethasone drops
thrice a day for two weeks for the inflamed pterygium.
Routine investigations performed were blood
complete picture, random blood sugar, renal function tests, and Urine routine
examination, which were all normal.
The crystals did not
interfere with vision, nor seemed infectious, so were not sought to be treated,
neither was the traumatic, crystalline cataract, which was not in the pupillary
area. The crystals were stable until the last follow-up.
DISCUSSION
Trees and plants with milky sap are a
common place. Such plants can be ornamental, or used in medicines or food.
About 12 families, 20 genera and more
than 5000 species of milky latex sap
occur in the world. The toxicity from the sap is attributed to essential oils,
alkaloids, amino acids, proteins, glycerides, plant acids, peptides, saponins,
terpenes, furano-coumarins, and poly-acetylene compounds. Local or oral use can
have profound toxic effects. Skin contact can lead to a blistering reaction,
while contact with eyes can cause a severe keratoconjunctivitis, uveitis, corneal
scarring and even permanent visual loss9,10.
Dieffenbachia plant typically has ejector pods containing raphides, which if
lightly squeezed, result in an explosive ejection2 of these
needle-like calcium oxalate crystals, which penetrate the corneal epithelium;
allowing further chemical injury by oxalic acid and plant proteins. This gun
like effect allows these crystals to penetrate deep into the cornea.
All the six species of the Araceae family1-4; Dieffenbachia, Arisaema and Colocasia, Alocasia, Pinellia, and
Phylodendron; reported previously to cause corneal crystals, are small
ornamental plants, but in this case, our patient was hit by a tall tree, whose
nature is obviously unknown to us; and could, but possibly does not belong to
this family; as these are small ornamental plants, and not at all tall. We
would have liked to identify the tree, but the injury occurred decades ago, in
the dark night, and the patient could not identify or recall the type of tree
at all, and also because of the severe symptoms caused by it, he was rushed to
a hospital. The offending plant caused a penetrating injury to the eye, resulting
in a full thickness corneal tear and the sap penetrated both the cornea and the
lens capsule as well, to cause crystallization in both the corneal stroma, and
also within the small, cortical cataract.
Although, plants from the Araceae family are found in Pakistan10,
it is difficult in this case to identify the offending plant.
Dieffenbachia typically causes fine, blue9, needle like crystals
within the corneal stroma, which resolve with topical steroid and antibiotic
therapy. Our patient had fine and silvery crystals, rather than needle-like,
which are probably not of the same nature as calcium oxalate. Deposition of
these crystals deep into the anterior lens cortex, also suggests an explosive
mechanism of ejection of plant sap, similar to the Dieffenbachia plant. The
crystals in our patient differ from other causes of crystalline keratopathy,
especially infectious; where the crystals are also needle like. Association of
the crystals to the corneal scar and cataract point to tree sap injury, rather
than other metabolic causes or drugs, which lead to bilateral deposits, and
have been ruled out on the basis of history and investigations.
Plant sap exposure is an extremely interesting
cause of corneal crystals, and in this case lenticular crystals as well; which
is unknown to many ophthalmologists, and must be kept in mind while evaluating
a patient who presents to us with corneal crystals. In addition, the
ophthalmologists need to be aware of the constituents of these milky sap plants
and their sequelae, in order to effectively treat such cases. The patients
should be asked to identify the culprit plant and bring the offending leaf with
them. Upon identification, it is important to report these plants in order to
increase awareness and prevent injury.
The need arises to wear protective glasses
and gloves while working in the garden, and to rinse the splashed areas
immediately, in the event of accidental exposure. Such patients with eye
exposure presenting to the hospital need to be irrigated with normal saline
immediately, followed by meticulous steroid and antibiotic therapy to suppress
keratoconjunctivitis, which in the majority of cases is self-limiting9.
In conclusion, crystals
in the eye have abundant causes, the common ones have been discussed frequently.
However, cataract inflicted by tree sap injury must also be
kept in mind while evaluating these cases.
REFERENCES
1.
Ellis W, Barfort P, Mastman GJ. Keratoconjunctivitis with corneal crystals caused by the
diffenbachia plant. Am J Ophthalmol. 1973 Jul; 76 (1): 143-147.
2.
Seet B, Chan WK, Ang CL. Crystalline keratopathy from Dieffenbachia plant sap. Br J
Ophthalmol. 1995; 79: 98-99.
3.
Tang EW, Law RW, Lai JS. Corneal injury by wild taro. Clin Exp Ophthalmol. 2006 Dec; 34 (9):
895-6.
4.
Hsueh KF, Lin PU, Lee SM, Hsieh CF. Ocular injuries from plant sap of genera Euphorbia and Dieffenbachia.
J Chin Med Assoc. 2004; 67 (2): 93-98.
5.
Gorovoy MS, Stern GA, Hood CI, Allen C. Intrastromal noninflammatory colonization of a corneal graft.
Arch Ophthalmol. 1983 Nov; 101 (11): 1749-52.
6.
Yanoff
M, Duker JS. Ophthalmology. Third Edition. Mosby: St. Louis, 2009: p 264.
7.
Porter AJ, Lee GA, Jun AS. Infectious crystalline keratopathy. Surv Ophthalmol. 2018
Jul-Aug; 63 (4): 480-499.
8.
Weiss JS, Khemichian AJ. Differential diagnosis of Schnyder crystalline dystrophy. Dev
Ophthalmol. 2011; 48: 67-96.
9.
Lembach RG, Ringel DM. Factitious bilateral crystalline keratopathy. Cornea, 1990 Jul; 9
(3): 246-8.
10.
Ahmad S. A
study of poisonous plants of Islamabad area, Pakistan. Pak J Sci Ind Res. Ser.
B. 2012; 55 (3): 129-137.